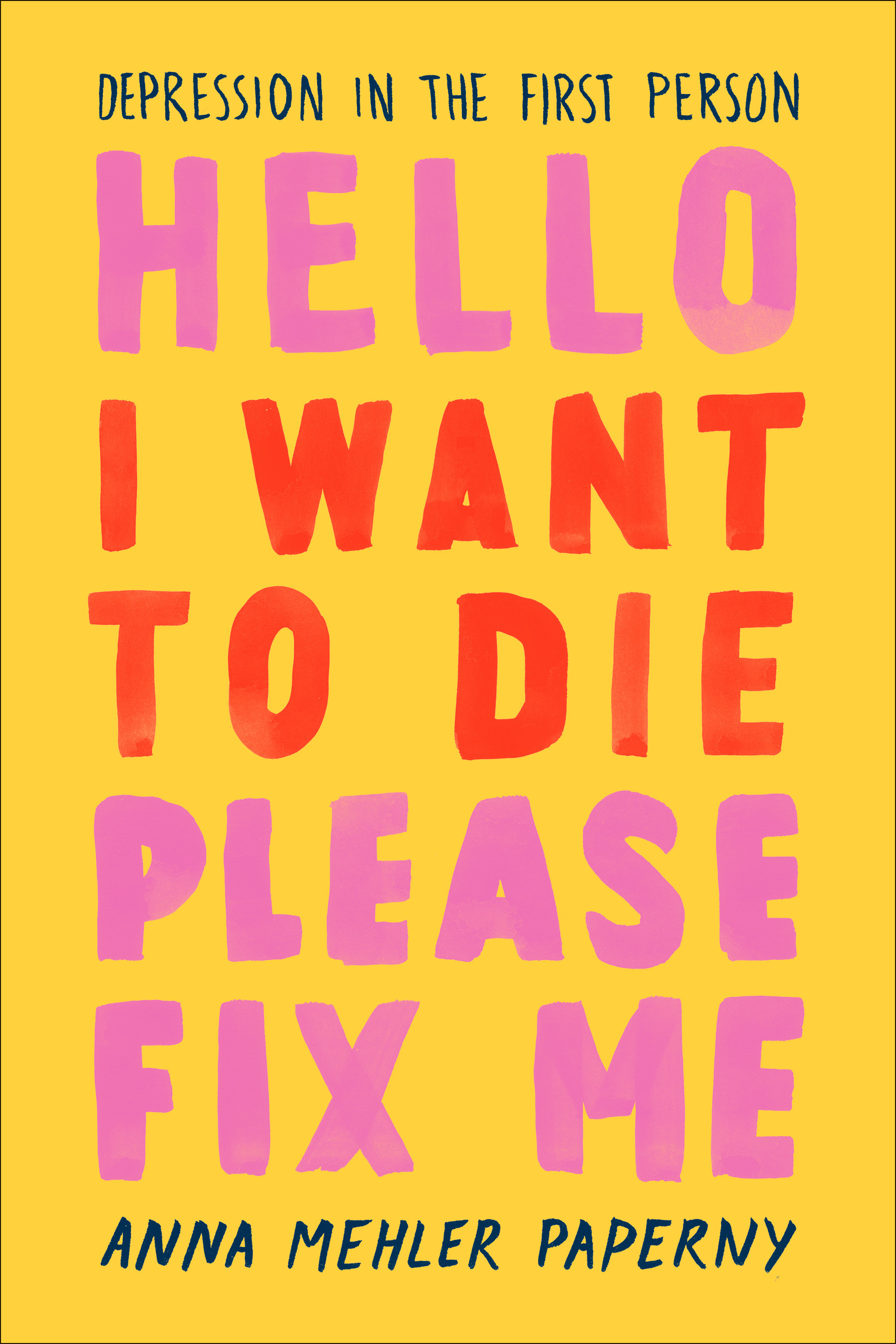
Hello I Want to Die Please Fix Me: Depression in the First Person
Anna Mehler Paperny
Questions & Answers
The author's personal experience with depression deeply informs the narrative and analysis of the broader mental health landscape. Her first-person account provides a raw, intimate perspective on the struggles of living with depression, including the complexities of diagnosis, treatment, and the emotional impact. This personal narrative serves as a powerful foundation for her exploration of the mental health system, highlighting the gaps and challenges faced by individuals like herself. Her insights into the limitations of current treatments, the stigma surrounding mental illness, and the systemic failures in mental health care are all informed by her lived experience, making her analysis both empathetic and critical. The author's journey also underscores the importance of personal agency and the need for systemic change, as she seeks to understand and overcome her own struggles while advocating for a more compassionate and effective mental health system.
The challenges and limitations of current mental health treatments, particularly for depression, include the high rate of treatment resistance, the lack of effective and accessible treatments, and the stigma associated with mental illness. Many patients do not respond to initial antidepressants, and treatment combinations often fail to provide lasting relief. The author highlights the need for better understanding of depression, improved treatment options, and increased funding for research.
To address these issues, the author proposes several solutions:
- Developing and validating biomarkers to identify specific treatment options for individual patients.
- Encouraging public funding for research to identify novel compounds and treatments.
- Creating multi-party partnerships to develop new treatments for conditions with high public interest.
- Addressing stigma by promoting awareness and understanding of mental illness.
- Improving access to mental health care, particularly for marginalized populations, and advocating for better support systems.
Stigma surrounding mental illness, especially depression, significantly impacts individuals and the broader mental health system. Individuals face discrimination, leading to isolation, reduced access to employment, and social exclusion. This stigma can also deter individuals from seeking help, exacerbating their conditions. For the mental health system, stigma leads to underfunding, insufficient resources, and a lack of trained professionals. It also hinders research and the development of effective treatments. The broader impact includes a higher prevalence of untreated mental illness, increased emergency room visits, and higher rates of suicide, ultimately burdening healthcare systems and society as a whole.
The author believes that technology and emerging treatments like deep brain stimulation (DBS) and psychedelic therapy could significantly transform mental health care. DBS, by implanting electrodes in the brain, holds promise for treating depression by correcting abnormal brain activity. The author also highlights the potential of psychedelic therapy, which has shown rapid antidepressant effects in some cases. These treatments could offer more personalized and effective care, potentially reducing the need for trial-and-error medication and psychotherapy. However, the author acknowledges the current limitations and the need for further research to refine these treatments and ensure their safety and efficacy.
The author argues for a more equitable and accessible mental health care system by highlighting the disparities and challenges faced by individuals with mental illness. Key points include:
- Universal Coverage: The author emphasizes the need for universal coverage of pharmacotherapy and psychotherapy, ensuring that mental wellness is not a privilege for the wealthy.
- Collaborative Care: Encouraging collaboration between primary care providers and psychiatrists to improve early detection and treatment.
- Biomarkers: Research into identifying specific biomarkers for individual patients to tailor treatments effectively.
- Digital Tools: Utilizing smartphones and digital tools for mental health monitoring and intervention, but with careful consideration of privacy and security.
- Zero Suicide Strategy: Implementing strategies to identify and support individuals at risk of suicide, including comprehensive screening and follow-up care.
- Addressing Stigma: Challenging the stigma surrounding mental illness and promoting open dialogue about mental health.
- Improving Inpatient Care: Making inpatient care more humane and patient-centered, focusing on building trust and empathy between patients and healthcare providers.
To achieve these goals, changes include increased funding for mental health services, better training for healthcare providers, and policy reforms to ensure equitable access to care.